AMA Manual of Style - Stacy L. Christiansen, Cheryl Iverson 2020
Cardiology
Nomenclature
Several areas of cardiology use simple letter terms and alphanumeric terms that do not need to be expanded at first mention.
14.3.1 Electrocardiographic Terms.
International standardization of electrocardiographic nomenclature dates back to the mid-20th century.1,2,3,4 The preferred abbreviation for electrocardiogram and electrocardiographic is ECG, not EKG. In the following examples of ECG terms, note the use of capitals, lowercase letters, subscripts, and hyphens.
14.3.1.1 Leads.
Leads (recording electrodes) are designated in Table 14.3-1.
Table 14.3-1. Types and Names of Electrocardiographic Leads
Types of leads |
Names |
standard (bipolar) leads |
I, II, III |
augmented limb leads/unipolar extremity leads (a, augmented; V, voltage; R, right arm; L, left arm; F, foot) |
aVR, aVL, aVF |
inverted aVR lead |
−aVR |
(unipolar) precordial (chest) leads |
V1, V2, V3, V4, V5, V6, V7, V8, V9 (eg, leads V3 through V6 [not V3-V6 or V3-6]) |
right precordial leads |
V1R, V2R, V3R, V4R, V5R, V6R |
modified chest lead using V1 |
MCL1 |
14.3.1.2 Deflections.
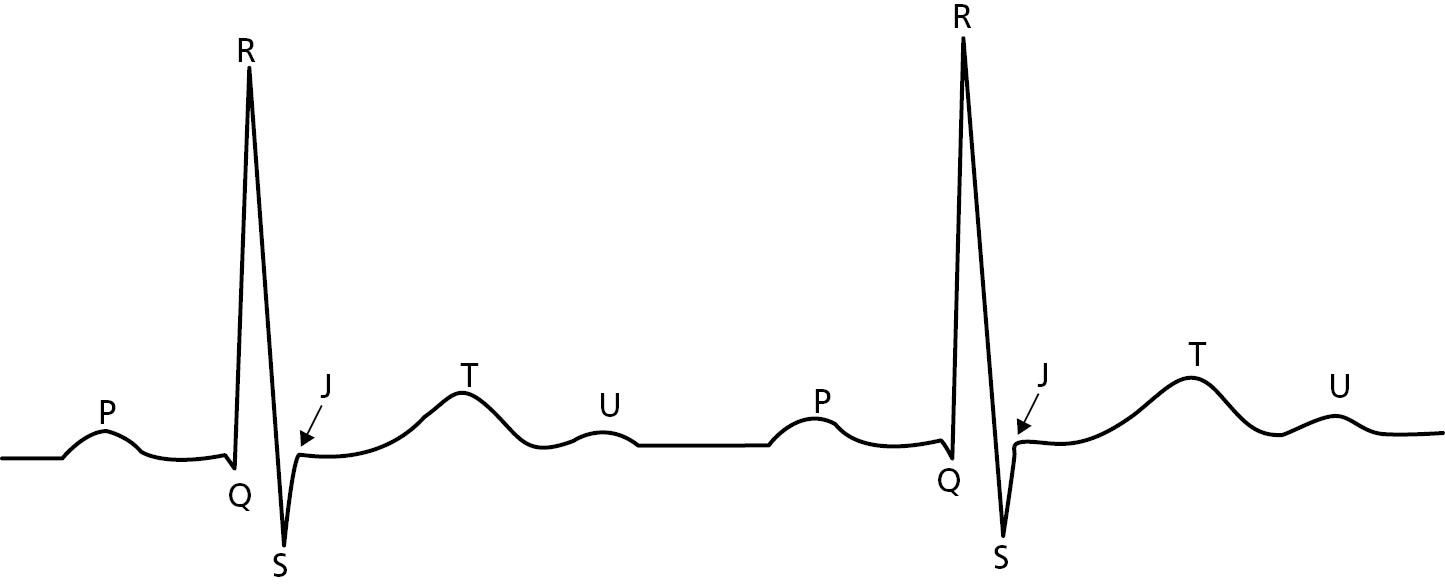
The main deflections of the ECG (Figure 14.3-1) are named in alphabetical sequence (P, Q, R, S, T, U), a usage that dates back to the inventor, Willem Einthoven.2 Other deflections use initial letters of the entity being described.
Capital letters are used to describe generic ECG deflections.
Improper paper speed during ECG recording will spuriously alter the QRS configuration [not qrs configuration].
In reference to an individual ECG tracing, or in descriptions of some specific ECG patterns, capital letters may indicate larger waves and lowercase letters smaller waves; in practice, this most often applies to the Q, R, and S waves.
Pathologic Q waves occur in myocardial infarction.
The q wave in aVF and the Rr′ pattern in lead V3 in this patient’s ECG were considered normal findings.
An rSR′ complex in the anterior chest leads and qRs in the left chest leads may indicate right bundle-branch block.
As a guide, hyphens usually do not link deflection terms in the same PQRSTU complex (eg, QT) but link deflections in different waves (eg, R-R), with the exception of ST-T. The following are examples of terms descriptive of deflections and patterns in ECG tracings:
delta wave (preferred over ∆ wave; a slurred upstroke in the QRS complex that is associated with a short PR interval)
F wave (atrial flutter wave)
f wave (atrial fibrillation wave)
J point, J junction (junction of QRS complex and ST segment)
J-ST axis, vector
LQTS (long QT syndrome)
NSTEMI (non—ST-segment elevation myocardial infarction)
NSTE ACS (non—ST-segment elevation acute coronary syndrome)
P wave, axis, etc
PR interval, segment, etc (not P-R)
Figure 14.3-1. Electrographic Deflections (Schematic)
Q wave, q wave
qR complex
QR-type complex
QRS complex (usually a combination of Q, R, and S waves), QRS configurations (if the QRS complex lacks an R wave, it is called a QS complex; if the QRS complex lacks a Q wave, it is called an RS complex)
QRS-T complex
QS wave, qs wave
QT interval, prolongation, etc (not Q-T)
QTc (corrected QT interval)
R wave, r wave, R′ wave, r′ wave
R-on-T
R-R interval
rS, RS, Rs complex, configuration, etc
R/S (ratio)
rSR′ pattern
S wave, s wave
S′ wave, s′ wave
ST segment, depression, axis, etc (not S-T)
ST-segment abnormality
ST-T segment, elevation, changes, axis, etc (not S-T-T)
STEMI (ST-segment elevation myocardial infarction)
T wave, axis, etc
Ta wave (atrial repolarization)
TQ segment
U wave
When terms such as the foregoing are used as modifiers, use a hyphen before the modifying noun (see 8.3, Hyphens and Dashes).
P-wave duration
Q-wave irregularity
non—Q-wave myocardial infarction
ST-segment depression (not S-T)
The following symbols are used in connection with ECGs obtained from patients with pacemakers:
A |
atrial stimulus |
V |
ventricular stimulus |
AV |
interval from atrial stimulus to succeeding ventricular stimulus |
AR |
interval from atrial stimulus to conducted spontaneous ventricular depolarization |
PV |
interval from spontaneous atrial depolarization to succeeding “atrial-synchronous” ventricular stimulus |
Lead and tracing terms may be combined to describe pattern and location together.
RI |
R wave in lead I |
RaVL |
R wave in aVL |
SIII |
S wave in lead III |
RV3 |
R wave in V3 |
S1Q3T3 pattern |
prominence of S wave in lead I, Q wave in lead III, and T-wave inversion in lead III |
SV1 + RV5 |
sum of voltages of S wave in V1 and R wave in V5 |
The P axis, QRS axis, ST axis, and T axis are specified with a plus or minus sign followed by the number of degrees in arabic numerals (eg, +60°, −30°).
14.3.2 Electrograms.
Electrogram (EGM) terms pertain to invasive electrophysiologic recording of cardiac impulse conduction. Expand these terms at first mention.
AH interval |
atrial-His interval |
His |
His potential |
HV interval |
His-ventricular interval |
14.3.3 Heart Sounds.
The 4 heart sounds and 4 components are commonly abbreviated in discussions of cardiac auscultatory findings; numerical subscripts are used.
S1 first heart sound
M1 mitral valve component
T1 tricuspid valve component
S2 second heart sound
A2 aortic valve component
P2 pulmonic valve component
S3 third heart sound
✵ The presence of an audible S3 was consistent with the patient’s ventricular aneurysm.
S4 fourth heart sound
✵ An audible S4 may be due to a variety of cardiac and systemic conditions.
Sound names may be written out in full when discussed generically.
Third heart sounds are suggestive of congestive heart failure, but an S3 gallop may be a normal finding in children and young adults.
or
The S3 is suggestive of congestive heart failure, but an S3 gallop may be a normal finding in children and young adults.
For plurals, follow the term with “sounds” or another noun.
S3 sounds [not S3s] may be normal or pathologic.
S3 gallops may be a normal finding in children and young adults.
14.3.4 Murmurs.
Murmurs are graded from soft (lower grade) to loud (higher grade). Murmur grades are written in arabic numerals. Systolic murmurs may be graded from 1 to 6 (see Freeman and Levine5) and diastolic from 1 to 4. Murmurs may also be presented by means of a virgule construction to indicate highest grade, as in the following examples:
grade 2 systolic murmur
grade 1 diastolic murmur
grade 4/6 systolic murmur
grade 2/4 diastolic murmur
The patient had a grade 3 systolic murmur radiating to the axilla consistent with the diagnosis of mitral valve regurgitation.
14.3.5 Jugular Venous Pulse.
The jugular venous pulse (JVP) contours are expressed with italic single letters and roman words:
a wave (atrial)
x descent
z point
c wave
x′ descent
v wave (ventricular)
y descent (or y trough)
h wave
Examples are as follows:
prominent a wave
giant a wave
steep x descent
increased v wave
abrupt y descent
14.3.6 Echocardiography.
The names of major echocardiographic methods are listed below. Expand any abbreviations at first mention.
2-dimensional echocardiography (2DE)
3-dimensional echocardiography (3DE)
4-dimensional echocardiography (4DE)
adenosine stress echocardiography
cardiac catheter echocardiography
color Doppler echocardiography
color flow Doppler echocardiography
continuous-wave Doppler echocardiography (CW Doppler)
contrast echocardiography
dipyridamole stress echocardiography
dobutamine stress echocardiography
Doppler echocardiography
Doppler flow imaging
exercise echocardiography
intravascular ultrasonography (IVUS)
pharmacologic stress echocardiography
pulsed Doppler echocardiography
spectral Doppler echocardiography
standard transthoracic echocardiography6 (a combination of 2-dimensional echocardiography, M-mode [motion mode], and Doppler flow imaging)
echocardiography, M-mode [motion mode], and Doppler flow imaging
stress echocardiography
transesophageal echocardiography (TEE)
The following commonly used echocardiographic indexes should also be expanded at first mention:
AVA |
aortic valve area |
EF |
ejection fraction |
EPSS |
E point septal separation |
FAC |
fractional area change |
FS |
fractional shortening |
IVS, IVST |
interventricular septal thickness |
LVID |
left ventricular internal dimension |
MVA |
mitral valve area |
PHT |
pressure half-time |
PW, PWT |
posterior wall thickness |
RVID |
right ventricular internal dimension |
SAM |
systolic anterior motion of the mitral valve |
d or ed |
end diastole |
s or es |
end systole |
Terms are combined as in the following examples:
IVSd |
interventricular septal thickness at diastole |
IVSs |
interventricular septal thickness at systole |
LVIDd |
left ventricular internal diameter at diastole |
LVIDed |
left ventricular internal diameter at the end of diastole |
LVIDes |
left ventricular internal diameter at the end of systole |
LVIDs |
left ventricular internal dimension at systole |
LVPWd |
left ventricular posterior wall dimension at diastole |
LVPWs |
left ventricular posterior wall dimension at systole |
RVIDd |
right ventricular internal dimension at diastole |
Ejection fraction (EF) is expressed as a percentage (eg, 60%) (see 18.0, Numbers and Percentages).
14.3.7 Pacemaker Codes.
The capabilities and operation of cardiac pacemakers are described by 3- to 5-letter codes.7,8
DDIR pacing
VVI pacemaker
The code system for antibradycardia pacemakers endorsed by the North American Society of Pacing and Electrophysiology (NASPE) and the British Pacing and Electrophysiology Group (BPEG) is known as the NASPE/BPEG Generic Code or NBG Code. Although the code need not be expanded when mentioned in passing, it is good practice to describe pacing modes in prose at first mention, for example, “dual-chamber, adaptive-rate (DDDR) pacing.” The NBG Code was revised in 2001 to apply to antibradycardia, adaptive rate, and multisite pacing.9,10
In Table 14.3-2, positions I through V refer to the first through fifth letters of the NBG Code. The character for “none” is the letter O, not the numeral 0. In practice, the first 3 positions are always given; the fourth and fifth are added when necessary to provide additional information.
Table 14.3-2. Revised North American Society of Pacing and Electrophysiology (NASPE)/British Pacing and Electrophysiology Group (BPEG) Generic Code for Antibradycardia Pacinga
Position |
I |
II |
III |
IV |
V |
Category |
Chamber(s) paced |
Chamber(s) sensed |
Response to sensing |
Rate modulation |
Multisite pacing |
O = none |
O = none |
O = none |
O = none |
O = none |
|
A = atrium |
A = atrium |
T = triggered |
R = rate modulation |
A = atrium |
|
V = ventricle |
V = ventricle |
I = inhibited |
V = ventricle |
||
D = dual (A+V) |
D = dual (A + V) |
D = dual (T + I) |
D = dual (A + V) |
||
Manufacturers’ designation only |
S = single (A or V) |
S = single (A or V) |
a Reproduced with permission from Bernstein et al.9
14.3.8 Implanted Cardioverter-Defibrillators.
A similar code, known as the NASPE/BPEG Defibrillator Code or NBD Code,11 exists for implanted cardioverter/defibrillators (ICDs), as defined in Table 14.3-3.
Table 14.3-3. Revised NASPE/BPEG Generic Code for Defibrillatorsa
Position I (shock chamber) |
Position II (antitachycardia pacing chamber) |
Position III (tachycardia detection) |
Position IV (antibradycardia pacing chamber) |
O = none |
O = none |
E = electrocardiogram |
O = none |
A = atrium |
A = atrium |
H = hemodynamic |
A = atrium |
V = ventricle |
V = ventricle |
V = ventricle |
|
D = dual (A + V) |
D = dual (A + V) |
D = dual (A + V) |
a Reproduced with permission from Bernstein et al.11
Examples are as follows:
DDH defibrillator
VOEO defibrillator
There is also a Short Form of the NBD Code intended only for use in conversation:
ICD-B |
ICD with antibradycardia pacing as well as shock |
ICD-T |
ICD with antitachycardia pacing as well as shock and antibradycardia pacing |
ICD-S |
ICD with shock capability only |
The foregoing terms can each represent a variety of devices; for instance, ICD-S could indicate VO, VOE, VOEO, DOH, or DOHV. The same devices may also be represented by more than 1 term; for instance, ICD-B may also represent VO and VOE, among other devices. Therefore, only the Long Form is used in writing. As in the case of the NBG Code, at first mention of an ICD it is good practice to include a prose description and the NBD Code designation.
For maximum conciseness and completeness in ICD labeling and record keeping, the first 3 positions of the NBD Code are given, followed after a hyphen by the first 4 positions of the NBG Code. Thus, VAE-DDDR refers to an ICD providing ventricular shock, atrial antitachycardia pacing, EGM sensing for tachycardia detection, and dual-chamber, adaptive-rate antibradycardia pacing.
14.3.9 Pacemaker-Lead Code.
The NASPE/BPEG Pacemaker-Lead Code (NBL Code)12 is detailed in Table 14.3-4.
Table 14.3-4. Revised North American Society of Pacing and Electrophysiology (NASPE)/British Pacing and Electrophysiology Group (BPEG) Pacemaker-Lead Codea
I (Electrode configuration) |
II (Fixation mechanism) |
III (Insulation material) |
IV (Drug elution) |
U = unipolar |
A = active |
P = polyurethane |
S = steroid |
B = bipolar |
P = passive |
S = silicone rubber |
N = nonsteroid |
M = multipolar |
O = none |
D = dual (P + S) |
O = none |
a Reproduced with permission from Bernstein and Parsonnet.12
Typically, all 4 positions are mentioned (eg, UPSO, BAPS).
Cardiac resynchronization therapy (CRT) devices, also known as biventricular devices, have additional functions and can be combined with implantable cardioverter-defibrillators, such as ICD/CRT, or can be stand-alone CRT devices.
14.3.10 Heart Disease Classifications and Scoring Systems.
Several classifications and scoring systems pertinent to heart disease are in use (Table 14.3-5).
Table 14.3-5. Heart Disease Classifications
Classification |
Applies to |
Classes |
Example |
Braunwald13 |
unstable angina |
I-III IA-IIIC |
Braunwald class I Braunwald class IIIB |
Canadian Cardiovascular Society (CCS)14,15 |
exertional angina |
I-IV |
CCS class II |
CHA2DS2-VASc score16 |
atrial fibrillation stroke risk |
Score of 0, low risk; ≥2, high risk; maximum score, 10 |
CHA2 DS2-VASc Score ≥2 |
Forrester17,18,19 |
cardiac function after myocardial infarction |
I-IV |
Forrester class I |
Global Registry of Acute Coronary Events (GRACE)20,21 |
acute coronary events |
ST-segment—elevation myocardial infarction; non—ST-segment—elevation myocardial infarction; unstable angina |
GRACE variables include ST-segment elevation and patient age |
Killip19,22,23 |
cardiac status after myocardial infarction |
I-IV |
Killip class I heart failure |
New York Heart Association (NYHA)24 |
cardiac disease and functional capacity |
I-IV |
NYHA class I |
Thrombolysis in Myocardial Infarction (TIMI)25 (eg, TIMI Risk Score, TIMI Grade Flow) |
acute coronary syndrome |
Score of 0-1, lowest risk; 6-7, highest risk |
TIMI score 0-1 |
The classes are assessed in various ways, for instance, by physical examination (Killip), hemodynamic measurement (Forrester), and patient history (NYHA). The detailed meanings of each class are beyond the scope of this book, but several style points may be noted:
■Severity increases from lower to higher numbers and letters.
■There is no automatic correspondence among classes (eg, Killip class I is not equivalent to NYHA class I).
■The numerals for the classes, unlike those for the scores, are designators and are not quantitative or semiquantitative. Therefore, roman numerals are appropriate for those, whereas arabic numerals are used for the scores. The scores are a sum of points for various components.
✵
Avoid: |
Forrester class >2 |
Preferred: |
Forrester class above II class greater than Forrester II Forrester classes III and IV |
■Authors should describe their classification criteria, for instance:
Killip class on admission was determined as the following: patients whose disease was considered class I were free of rales and a third heart sound; patients whose disease was class II had rales up to 50% of each lung field regardless of the presence of the third heart sound. . . (adapted from Neskovic et al26).
We suggest that cases of unstable angina class IIIB now be subdivided into troponin-positive and troponin-negative subgroups. . . (adapted from Hamm and Braunwald27[p120]).
14.3.11 Coronary Artery Angiographic Classifications.
Guidelines are available for nomenclature of coronary artery segments,28 used in coronary artery catheterization and thrombolysis in myocardial infarction flow (TIMI flow).
The TIMI flow is expressed as grade 0, grade 1, grade 2, or grade 3, from lowest flow (or severest lesion) to highest flow.27
14.3.12 Cellular and Molecular Cardiology.
14.3.12.1 Cardiac Muscle.
These descriptive terms do not require expansion:
A band |
actin-myosin overlap |
H band |
Hensen (discoverer) |
M line |
mesophragma |
T tubules |
tubulus transversus |
Z line |
Zückung (German: “contraction”) |
Expand these terms at first mention:
TnC |
troponin C (binds calcium) |
TnI |
troponin I (inhibits actin-myosin interactions) |
TnT |
troponin T (binds to tropomyosin) |
cTnC |
troponin C, cardiac form |
cTnI |
troponin I, cardiac form |
cTnT |
troponin T, cardiac form |
hsTn |
high-sensitivity troponin |
14.3.12.2 Lipoproteins and Related Terms.
Expand the following lipoproteins and related terms at first mention:
acyl CoA |
acyl coenzyme A |
HDL |
high-density lipoprotein |
HDL1 |
HDL variant |
HDL2 |
HDL subfraction 2 |
HDL3 |
HDL subfraction 3 |
HDL-C |
HDL cholesterol |
HDL-R |
HDL receptor |
HMG-CoA |
3-hydroxy-3-methylglutaryl coenzyme A |
IDL |
intermediate-density lipoprotein |
IDL-C |
IDL cholesterol |
IDL-R |
IDL receptor |
LDL |
low-density lipoprotein |
LDL-C |
LDL cholesterol |
LDL-P |
LDL particle number |
LDL-R |
LDL receptor |
Lp(a) |
lipoprotein a |
LPL |
lipoprotein lipase gene (see 14.6.2, Human Gene Nomenclature) |
LPL188 |
mutation in LPL at codon 188 (see 14.6.1, Nucleic Acids and Amino Acids) |
LPLAsn29Ser |
substitution in LPL of serine at asparagine residue 29 |
LP-X |
lipoprotein X |
LRP1 |
LDL-R—related protein |
LRP2 |
LDL-R—related protein 2 |
VHDL |
very high-density lipoprotein |
VLDL-C |
VLDL cholesterol |
VLDL-R |
VLDL receptor |
Expand apo as apolipoprotein at first mention of terms such as the following:
apo AI |
apo B48 |
apo CI |
apo D |
apo E |
apo J |
apo AII |
apo B100 |
apo CII |
apo E2 |
||
apo AIII |
apo CIII |
apo E3 |
|||
apo AIV |
|||||
apo(a) |
|||||
apo AIMilano |
|||||
|
apo AIArg173Cys (substitution of cysteine at arginine 173 residue) (see 14.6.1, Nucleic Acids and Amino Acids) |
|||||
14.3.12.3 Miscellaneous Cellular and Biochemical Terms.
If an expansion is given, use at first mention. Otherwise, terms may be used without expansion.
athero-ELAM |
endothelial leukocyte adhesion molecule involved in atherosclerosis |
BNP |
B-type natriuretic peptide |
CK-MB |
creatine kinase, myocardial (largely considered obsolete as a test for myocardial infarction; replaced by troponin [Tn]) |
NOS |
nitric oxide synthase |
NOS1 |
neuronal NOS (named in order of discovery, also nNOS |
NOS2 |
also iNOS (inducible NOS) |
NOS3 |
also eNOS, ecNOS (endothelial constitutive isoform of NOS) |
P cell |
nodal cells of the sinus node |
tPA |
tissue plasminogen activator |
Principal Author: Cheryl Iverson, MA
Acknowledgment
Thanks to the following for reviewing and providing comments: Philip Greenland, MD, JAMA, and Northwestern University, Chicago, Illinois; Eric D. Peterson, MD, MPH, JAMA, and Duke University School of Medicine, Durham, North Carolina; Rita F. Redberg, MD, MSc, JAMA Internal Medicine, and Women’s Cardiovascular Services, University of California, San Francisco; Rochelle C. Lodder, formerly with JAMA Network; and Philip Sefton, MS, ELS, JAMA. Thanks also to David Song, JAMA Network, for obtaining permissions.
References
1.Barnes AR, Pardee HEB, White PD, Wilson FN, Wolferth CC; Committee of the American Heart Association for the Standardization of Precordial Leads. Standardization of precordial leads: supplementary report. Am Heart J. 1938;15(2):235-239.
2.Barnes AR, Katz LN, Levine SA, Pardee HEB, White PD, Wilson FN. Report of the Committee of the American Heart Association on the Standardization of Electrocardiographic Nomenclature. Am Heart J. 1943;25(4):528-534.
3.Barnes AR, Pardee HEB, White PD, Wilson FN, Wolferth CC. Second supplementary report by the Committee of the American Heart Association for the Standardization of Precordial Leads. Am Heart J. 1943;25(4):535-538.
4.Wilson FN, Kossmann CE, Burch GE, et al. Recommendations for standardization of electrocardiographic and vectorcardiographic leads. Circulation. 1954;10(4):564-573.
5.Freeman AR, Levine SA. The clinical significance of the systolic murmur: a study of 1000 consecutive “non-cardiac” cases. Ann Intern Med. 1933;6(11):1371-1385.
6.Mann DL, Zipes DP, Libby P, Bonow RO. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 10th ed. Elsevier Saunders; 2014.
7.Bernstein AD, Camm AJ, Fletcher RD, et al. The NASPE/BPEG Generic Pacemaker Code for antibradyarrhythmia and adaptive-rate pacing and antitachyarrhythmia devices. Pacing Clin Electrophysiol. 1987;10(4, pt1):794-799. doi:10.1111/j.1540-8159.1987.tb06035.x
8.Parsonnet V, Furman S, Smyth NPD. Implantable cardiac pacemakers status report and resource guideline: Pacemaker Study Group. Circulation. 1974;50(4):A21-A35.
9.Bernstein AD, Daubert J-C, Fletcher RD, et al. The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. PACE. 2002;25(2):260-264. doi:10.1046/j.1460-9592.2002.00260.x
10.Bernstein AD, Camm AJ, Furman S, Parsonnet V. The NASPE/BPEG codes: use, misuse, and evolution. Pacing Clin Electrophysiol. 2001;24(5):787-788. doi:10.1046/j.1460-9592.2001.00787.x
11.Bernstein AD, Camm AJ, Fisher JD, et al. North American Society of Pacing and Electrophysiology Policy Statement: the NASPE/BPEG Defibrillator Code. Pacing Clin Electrophysiol. 1993;16(9):1776-1780. doi:10.1111/j.1540-8159.1993.tb01809.x
12.Bernstein AD, Parsonnet V. The NASPE/BPEG pacemaker-lead code (NBL Code). Pacing Clin Electrophysiol. 1996;19(11, pt 1):1535-1536. doi:10.1111/j.1540-8159.1996.tb03177.x
13.Braunwald E. Unstable angina: a classification. Circulation. 1989;80(2):410-414. doi:10.1161/01.CIR.80.2.410
14.Campeau L. Grading of angina pectoris. Circulation. 1976;54(3):522-523. doi:10.1161/01.CIR.54.3.522.b
15.Campeau L. The Canadian Cardiovascular Society grading of angina pectoris revisited 30 years later. Can J Cardiol. 2002;18(4):371-379.
16.Lip GYK, Nieuwlaat R, Pisters R, Lane DA, Crijns HGM. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial-fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137(2):263-272. doi:10.1378/chest.09-1584
17.Forrester JS, Diamond G, Chatterjee K, Swan HJC. Medical therapy of acute myocardial infarction by application of hemodynamic subsets (first of two parts). N Engl J Med. 1976;295(24):1356-1362. doi:10.1056/NEJM197612092952406
18.Forrester JS, Diamond GA, Swan HJC. Correlative classification of clinical and hemodynamic function after acute myocardial infarction. Am J Cardiol. 1977;39(2):137-145. doi:10.1016/S0002-9149(77)80182-3
19.Madias JE. Killip and Forrester classifications: should they be abandoned, kept, reevaluated, or modified? Chest. 2000;117(5):1223-1226. doi:10.1378/chest.117.5.1223
20.Granger CB, Goldberg RJ, Dabbous OH, et al; Global Registry of Acute Coronary Events Investigators. Predictors of hospital mortality in the Global Registry of Acute Coronary Events. Arch Intern Med. 2003;163(19):2345—2353. doi:10.1001/archinte.163.19.2345
21.Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ. 2006;333(7578):1091. doi:10.1136/bmj.38985.646481.55
22.Killip T, Kimball JT. Treatment of myocardial infarction in a coronary care unit: a two year experience with 250 patients. Am J Cardiol. 1967;20(4):457-464. doi:10.1016/0002-9149(67)90023-9
23.Werns SW, Bates ER. The enduring value of Killip classification. Am Heart J. 1999;137(2):213-215. doi:10.1053/hj.1999.v137.93200
24.Dolgin A; Criteria Committee of the New York Heart Association. Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels. 9th ed. Little Brown & Co; 1994:254.
25.Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284(7):835-842. doi:10.1001/jama.284.7.835
26.Neskovic AN, Otasevic P, Bojic M, Popovic AD. Association of Killip class on admission and left ventricular dilatation after myocardial infarction: a closer look into an old clinical classification. Am Heart J. 1999;137(2):361-367. doi:10.1053/hj.1999.v137.89744
27.Hamm CW, Braunwald E. A classification of unstable angina revisited. Circulation. 2000;102(1):118-122. doi:10.1161/01.CIR.102.1.118
28.Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography). J Am Coll Cardiol. 1999;33(6):1756-1824. doi:10.1016/S0735-1097(99)00126-6